Report: 30% Of Antibiotic Prescriptions Are Unnecessary
While the beef, pork, and poultry industries have been heavily criticized for using the large majority of antibiotics sold in the U.S. to fatten up their animals, that doesn’t mean that American physicians are being terribly judicious about the antimicrobials they prescribe. A new report shines a light on just how many antibiotic prescriptions are unnecessary, increasing the risk of developing drug-resistant superbugs.
The report [PDF] from the Pew Charitable Trusts and the Centers for Disease Control and Prevention surveys the use of antibiotics in outpatient medicine and turns up some troubling numbers.
 For example, the analysis found that 30% of all antibiotic prescriptions written following outpatient office visits were unnecessary. That equates to nearly 50 million unwarranted prescriptions a year in the U.S. alone.
For example, the analysis found that 30% of all antibiotic prescriptions written following outpatient office visits were unnecessary. That equates to nearly 50 million unwarranted prescriptions a year in the U.S. alone.
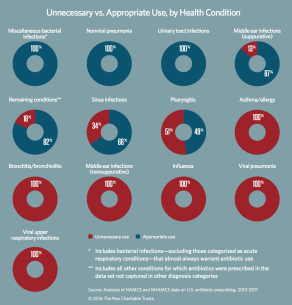
Prescriptions are frequently written for acute respiratory conditions like bronchitis, pharyngitis, asthma, allergies, and influenza. Many of these conditions will not respond to antibiotics, meaning the drugs are just going to waste. Click the chart at left to see the report’s breakdown on which conditions are receiving the most inappropriate prescriptions.
This data backs up a recent study which found 71% of doctors are still writing unhelpful prescriptions for acute bronchitis, even though healthcare industry guidelines have long stated that antibiotics should not be prescribed to patients whose only ailment is acute bronchitis.
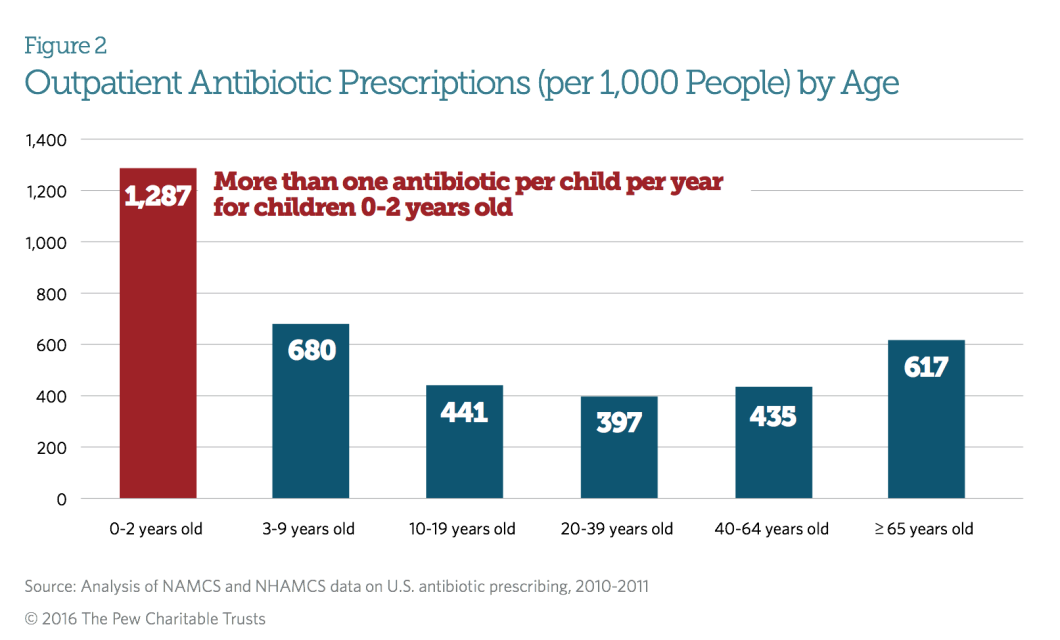
Little Kids; Lots Of Antibiotics
When looking at the age breakdown for antibiotics prescriptions, kids under the age of ten are being prescribed these drugs at the highest rates. In fact, children ages 2 and under are averaging more than one antibiotic prescription per child per year. That declines by nearly half for children ages 3 through 9, with nearly 7-in-10 children being prescribed an antibiotic each year.
Just The Tip Of The Drugberg?
While the Pew report accounts for millions of prescriptions written during outpatient visits to doctors’ offices, it does not include data for increasingly popular settings like retail clinics, urgent care facilities, and telemedicine. It also does not include data from dentists, who represent around 9% of all outpatient antibiotics prescriptions. Nor is the report able to factor in the prescribing done by physician assistants and nurse practitioners.
As such, the report’s authors note that the recommendations made regarding specific reductions of antibiotics use should be treated as a minimum if the U.S. is going to reach its goal of cutting overuse in half by 2020.
“The more antibiotics are used, the less effective they become. Reducing the needless use of antibiotics will slow the emergence of antibiotic-resistant microbes, so-called superbugs, which are among the most urgent public health threats of our time,” said Kathy Talkington, director of Pew’s antibiotic resistance project. “Patients and health care providers must work together to understand when antibiotics will help and when they won’t, and help preserve these lifesaving drugs for patients who really need them.”
More Than Superbugs
Antibiotics overuse isn’t just a case of wasted pills and money; overprescribed antibiotics can do more harm than good. In addition to concerns about encouraging the development of drug-resistant bacteria, antibiotics overuse can also lead to a colon infection from Clostridium difficile bacteria, resulting in potentially lethal diarrhea.
According to the report, half a million people a year fall ill with this infection, with 15,000 of them dying. In all, it’s estimated that more than 140,000 Americans head to the emergency room each year because of adverse events related to antibiotics.
“Prescribing unnecessary antibiotics is just one element of inappropriate use of antibiotics,” said Lauri Hicks, D.O., director of the CDC’s Office of Antibiotic Stewardship in the Division of Healthcare Quality Promotion. “Healthcare providers can also prescribe antibiotics at the wrong dose or for the wrong duration, amplifying the extent of inappropriate use. Setting a national target to reduce unnecessary antibiotic use is the first step, and we must work together across the health care continuum to reach this goal.”
Want more consumer news? Visit our parent organization, Consumer Reports, for the latest on scams, recalls, and other consumer issues.