 Image courtesy of C x 2
Image courtesy of C x 2
Doctors Finally Prescribing Fewer Antibiotics, But Continue Prescribing Unnecessary Antibiotics
A new report shows that overall antibiotic prescriptions are down 9%, but 1-in-5 antibiotics prescriptions aren't doing any patients any good.
A new report claims that American doctors may finally be heeding the message that public health regulators and advocates have been pushing for decades: Don’t respond to every cough, fever, or sore throat with a prescription for antibiotics. According to the report, antibiotics prescriptions appear to be on the decline, though physicians are still prescribing these drugs in cases where they aren’t helpful, and may actually cause harm.
Overuse of antibiotics is problematic in a number of ways. It encourages the development of drug-resistant bacteria, rendering current forms of treatment ineffective. Antibiotics like vancomycin that were once considered drugs of last resort have seen dramatic increases in use over the last decade as treatment options have dwindled. More than 2 million Americans fall ill from antibiotic-resistant infections each year, accounting for around 23,000 deaths annually, according to the Centers for Disease Control and Prevention.
Drug resistance isn’t some statistical anomaly. A 2014 survey by our colleagues at Consumers Union found that 85% of physicians had treated at least one patient in the previous year for an infection that was resistant to multiple classes of antibiotics.
In addition to the public health concern posed by antibiotics overuse, the practice can also have dire personal consequences. Taking too many antibiotics can lead to a colon infection from Clostridium difficile bacteria, resulting in potentially lethal diarrhea. The CDC says that some 15,000 people die each year as a result of C. difficile infections.
Despite scientific evidence, first-hand experience with resistance, and years-long campaigns by the CDC and public health advocates, some doctors continued to prescribe medically unnecessary antibiotics.
A 2016 report from Pew Charitable Trusts found that 30% of outpatient antibiotics prescriptions in the U.S. were not medically warranted — largely for for acute respiratory conditions like bronchitis, pharyngitis, asthma, allergies, and influenza. Many of these conditions will not respond to antibiotics, because the ailment is not caused by bacteria.
Speaking of acute bronchitis, the Healthcare Effectiveness Data and Information Set — performance measures used by the healthcare and insurance industry — has long stated that patients with just acute bronchitis should never be treated with antibiotics. But in 2014, the CDC noted that more than 70% of U.S. physicians were still treating this ailment with antibiotics they know (or should know) won’t help.
Declining Use
This message may finally be getting through to physicians and patients, according to new data from the Blue Cross Blue Shield Association which found that overall antibiotics prescription levels declined between 2010 and 2016.
The BCBS report, based on 173 million claims by 31 million of the insurers’ policyholders, concludes that there was a notable decline in the rate of antibiotics prescriptions over the seven-year period.
In 2010, BCBS was filling around 91 antibiotics prescriptions per 100 patients. By 2016, that had dropped to a little less than 83 antibiotics prescriptions per 100 patients.
While this drop in overall antibiotics use is a positive sign and may indicate improved awareness of the potential risks associated with overuse of these drugs, the report still highlights a number of causes for concern.
Pointless Prescriptions
According to the BCBS report, 21% of the antibiotics prescriptions written in 2016 were for conditions where the use of antibiotics is pointless. (Click image at right for charts.)
These include allergies, asthma, viral bronchitis, COPD, flu, and viral pneumonia. And three times as many antibiotics prescriptions were written in cases where it wasn’t known at the time whether antibiotics would help or if the cause of the illness was bacterial.
Going Too Broad
Even more troubling: The overwhelming majority (75%) of the medically unnecessary antibiotics prescriptions were for what’s known as “broad-spectrum” antibiotics. These are drugs used to treat a wide variety of possible bacterial infections.
Broad-spectrum antibiotics are helpful in cases where a patient needs to be treated immediately but the doctor doesn’t yet know exactly which type of bacteria is causing the infection. However, overuse of broad-spectrum drugs can result in a wider range of drug-resistant pathogens, so it’s not wise to use these antibiotics too frequently — and definitely not on patients where the drug won’t do any good.
BCBS says that broad-spectrum drugs are by far the most popularly prescribed antibiotics for outpatient care (the report did not include data on inpatient prescriptions), with nearly 44 broad-spectrum prescriptions being written for every 100 patients. That rate is down from more than 50 per 100 in 2010, but still more than 150% the rate of intermediate-spectrum antibiotics.
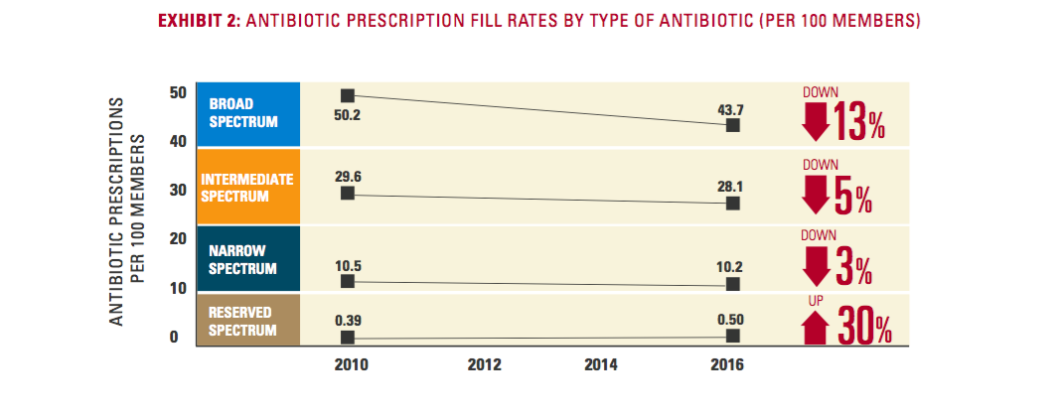
At the same time, “reserved-spectrum” antibiotics — the drugs of last resort like vancomycin — saw an increase of 30% over the seven-year period of the report. While the rate is still incredibly low (less than 1 prescription per 100 patients) in comparison to the other types of antibiotics, the increasing use of these drugs — coupled with the fact that these sorts of drugs have historically been used primarily for inpatient treatment — may indicate that physicians are more frequently seeing drug-resistant infections that won’t respond to other, more common antibiotics.
Regional Issues
Though the general rate of antibiotics prescription is down, the rate varies widely by region, with several southern and southeastern states having significantly higher rates than the national level.
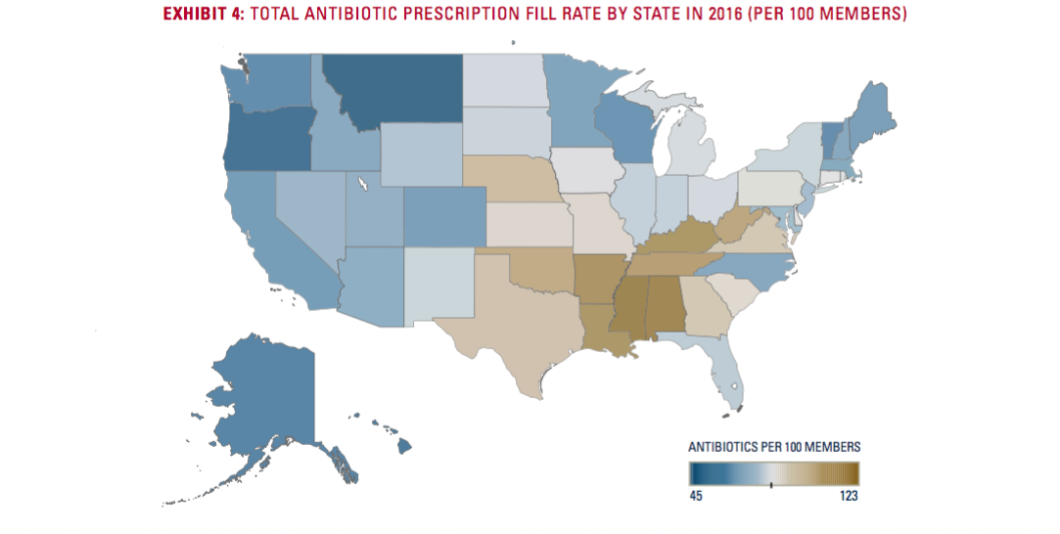
Eight states — Mississippi, Alabama, Arkansas, Kentucky, Louisiana, Tennessee, West Virginia, and Oklahoma — have antibiotics prescribing rates in excess of 100 prescriptions per 100 patients, with Mississippi (123.3) and Alabama (122.8) having the highest rates in the country.
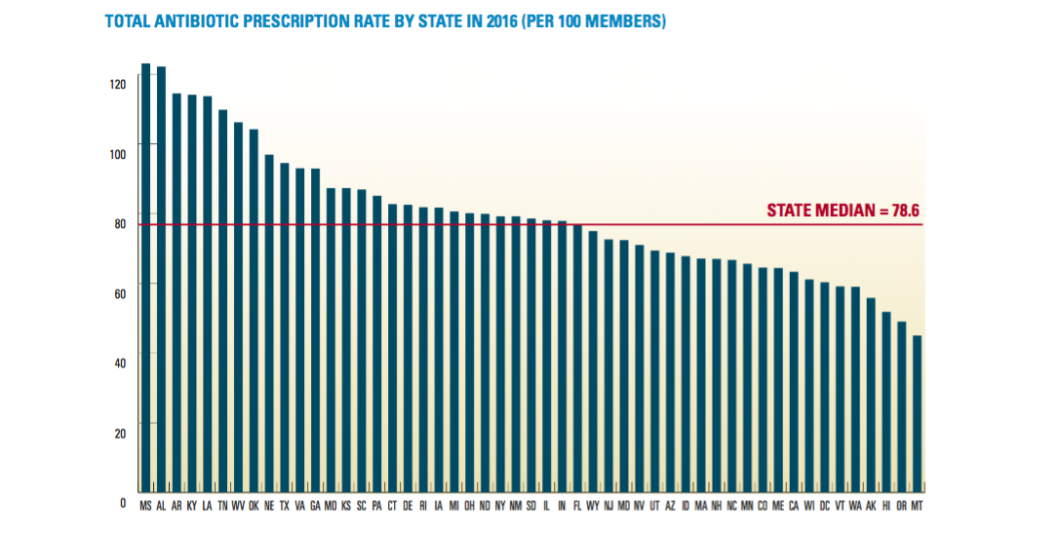
The silver lining in these numbers is that antibiotics prescribing rates have declined since 2010 in each of these states. Both Tennessee and West Virginia saw declines (12% and 13%, respectively) that were better than the 9% average decline for all states.
In fact, only two states — Delaware and Illinois — saw their prescribing rates go up during the seven-year period (3% increases in both cases). Nebraska’s rate remained unchanged.
Why Do Doctors Prescribe Unnecessary Antibiotics?
There’s no reason for a physician in the U.S. to not be aware of the link between overuse of antibiotics and drug-resistant bacteria, so why do some continue to write prescriptions for antibiotics that won’t help anyone?
One study out of Iceland attempted to identify the many factors at play in a physician’s decision to write a pointless prescription. Patient pressure was the most frequently cited cause in that study, and some doctors admitted that writing the antibiotics prescription was sometimes just a way to get through their day.
“I don’t like to argue with people and disagree with them… if they feel they’re right in some degree, somehow I don’t argue with them about it,” said one doctor in response to that study. “Even if I think I’m right. So I back down by issuing a prescription, in some cases.”
Others said they feared losing patients to doctors who would fulfill the patient’s wish for antibiotics, and that insistent patients are eventually going to find someone who will write that prescription.
It certainly can’t help when some companies reinforce the public’s misconceptions about antibiotics — like the pharmacy delivery startup that advertised “very, very strong antibiotics” for people who had been simply been near someone else who sneezed.
There’s also a sense of “I’m not the problem” among some doctors. A 2014 study from researchers at Children’s Hospital of Philadelphia also found that even though most pediatric physicians agree that overuse of antibiotics is a vital public health concern, many were dismissive that pediatricians were contributing to the problem by overprescribing antibiotics. Instead, these doctors blamed the overprescribing on non-pediatric care providers like emergency rooms and “quickie clinics.”
At the same time, nearly all of these same pediatric doctors surveyed for the study admitted they had “caved” to parental pressure and prescribed antibiotics despite deeming them unnecessary, particularly during cold and flu season.
“Honestly, I think some patients do get antibiotics just because we are running behind when we don’t have time to explain to parents why they aren’t necessary,” admitted one physician.
Want more consumer news? Visit our parent organization, Consumer Reports, for the latest on scams, recalls, and other consumer issues.

