Anthem Blue Cross Blue Shield Approves Cardiac Rehab Stay Fit For A Time Traveler
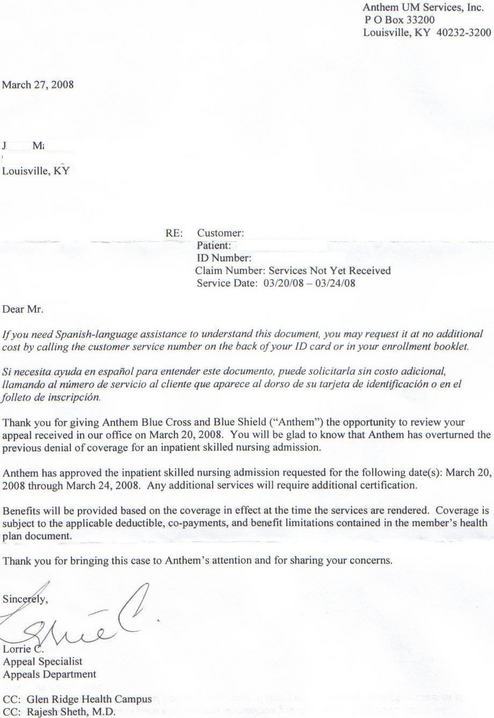
In a letter dated March 27, Anthem Blue Cross Blue Shield informed Dona that her father was approved to stay in a cardiac rehab center through March 24. Dona’s mother began planning for her husband’s care shortly before his triple-bypass on March 15. Anthem originally approved the off-site rehab, but changed its mind on March 19, the day before Dona’s father was scheduled to be discharged. With the support of his doctors, he filed an emergency appeal so he could move to rehab the next day. The retroactive approval arrived a week later.
On March 15, my dad had triple-bypass heart surgery at Jewish Hospital in Louisville, Kentucky. My mother immediately started planning for his aftercare. My mother is disabled and uses a walker to get around; my father normally takes care of her.
My father’s doctors, along with the hospital’s case worker and my mother tried to get their health insurer, Anthem Blue Cross/Blue Shield to approve off-site cardiac rehab. They initially approved the request and made arrangements at an approved facility. The day before checkout, March 19, Anthem changed it’s mind. My father’s doctors kept him another day to execute an emergency appeal. But to no avail, Anthem determined my father was “too healthy” and would have to go home (and basically perform self-care). It pushed my mother to the verge of a nervous breakdown, but thanks to friends and neighbors they made it work. Anthem was kind enough to provide a visiting nurse, three times a week, even though daily care was recommended by the doctors.
Yesterday, they received the attached letter, approving the rehab stay. Well, great, right? Let’s go to rehab! Well, no-no-no. The approval was only good until 3/24. So, he’ll have to re-apply.
Want more consumer news? Visit our parent organization, Consumer Reports, for the latest on scams, recalls, and other consumer issues.

